A version of this article was previously published in the November 2017 issue of Healthcare News.
 Hospitals across the country have seen many changes in the past seven years as the Affordable Care Act (ACA) has evolved and states have implemented various optional components of the legislation.
Hospitals across the country have seen many changes in the past seven years as the Affordable Care Act (ACA) has evolved and states have implemented various optional components of the legislation.
Under the ACA, many states have expanded their Medicaid coverage, attempted to roll out exchanges for commercial plans, or both. These changes have required the Centers for Medicare and Medicaid Services (CMS) to begin modifying certain payment methods to hospitals to redirect funds from their prospective payment systems to pay for the expansion of coverage in other areas of federal and state spending.
The Challenge
Exchange programs and changes to employer-based health plans had the intended effect of providing or modifying coverage for many individuals, changing the category of these patients from uninsured to insured.
However, although now technically insured, a large number of these individuals have high-deductible health plans (HDHPs), which have deductibles that often exceed $4,000. This high deductible level essentially places individuals who have difficulty making their premium payments—and consequently may qualify for financial assistance to meet these obligations—in the self-pay or charity care category.
One of the biggest challenges with this influx of insured individuals who still qualify for charity care is the process by which CMS determines hospital reimbursement payments.
Disproportionate-Share Hospitals (DSHs)
DSHs serve a disproportionate number of low-income and uninsured patients and receive payments from CMS to help cover some of these costs. Under the ACA, the calculation of these payments has changed to account for the expansion of Medicaid on a state-by-state basis and coverage on the exchanges nationwide.
Previously, Medicare handled DSH payments as an add-on to the payment for inpatient services using a threshold calculation of the hospital’s Supplemental Security Income (SSI) ratio and the percentage of Medicaid days to total patient days.
Under the ACA, the algorithm was modified to take the previous pool of DSH funds and redistribute them in the following manner:
- 25%—referred to as the empirical DSH payment—is still handled as an add-on to each claim using the prior methodology and settled on the hospital’s annual Medicare cost report
- 75% is distributed to the same population of hospitals based on factors that account for the change in the uninsured population nationwide as well as hospital-specific data
Uninsured Patients
Under the ACA, the federal government uses the number of uninsured patients—which has steadily declined since 2014—to determine the amount that needs to be diverted from the uncompensated-care pool to other programs under the ACA.
The table below illustrates the direct relationship between the uncompensated-care pool available for distribution and the percentage of uninsured patients nationwide as measured by the Congressional Budget Office.
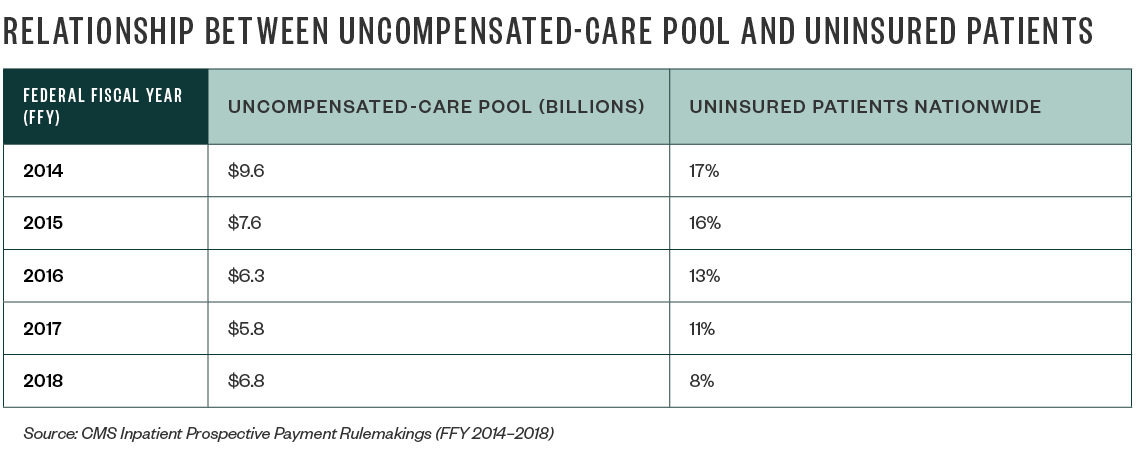
In many cases, the change in the uninsured rate was related to HDHP and Medicaid-plan expansion. This meant that although more patients were insured, hospitals were being reimbursed at lower rates compared to the cost of patient care—or receiving no payment at all in the case of charity care and other bad debt.
Medicaid Expansion
Compounding this issue is the fact that several states have opted not to expand their Medicaid program. Due to this policy decision, these states continue to see an increasing number of uninsured patients in their communities. For example, the rate of uninsured patients in Texas is nearing 19.5% in 2017—far above the 11% uninsured rate nationwide—and certain areas of the state are at even higher rates.
States with the Highest Uninsured Patient Rates
- Texas
- Oklahoma
- Alaska (recently expanded its Medicaid coverage)
- Georgia
- Mississippi
In the first few years of the new uncompensated-care-pool distribution, hospitals in expansion states realized a small benefit from increased Medicaid plan reimbursements because of a swell in patients who were previously uninsured but became eligible for Medicaid. This resulted in an increase in DSH reimbursements as the ratio of their Medicaid patients grew as a percentage of their total patient population.
Hospitals in the nonexpansion states listed above didn’t realize the same benefit because the payments depended on an expanded Medicaid population.
Medicare Cost Report Worksheet S-10
In federal fiscal years 2013 through 2017, the distribution of the uncompensated-care pool to eligible hospitals was driven by a calculation of the hospital’s Medicaid days and Supplemental Security Income (SSI) days compared to the national average.
This calculation wasn’t dramatically different from the historical settlement calculation of DSH dollars on each hospital’s annual Medicare cost report, but it allowed CMS to account for the reduction in the number of uninsured patients in the overall amount paid before distributing the remainder of the pool.
Beginning in federal fiscal year 2018, CMS added a third element to the hospital-specific calculation: calculated uncompensated-care cost from each eligible hospital’s Worksheet S-10. It’s important to note that CMS is only using the uncompensated-care cost calculated from the cost report, which doesn’t include the shortfall from Medicaid programs—another section of Worksheet S-10.
This lack of inclusion of the Medicaid shortfall creates issues for hospitals in states that expanded their Medicaid program. While expansion decreased their uninsured populations, the amount of reimbursement received from Medicaid plans falls far short of the cost of patient care. And with the new calculation, more money will be diverted from the uncompensated-care pool to hospitals with high charity care costs due to uninsured patient populations—an ancillary benefit for hospitals located in nonexpansion states.
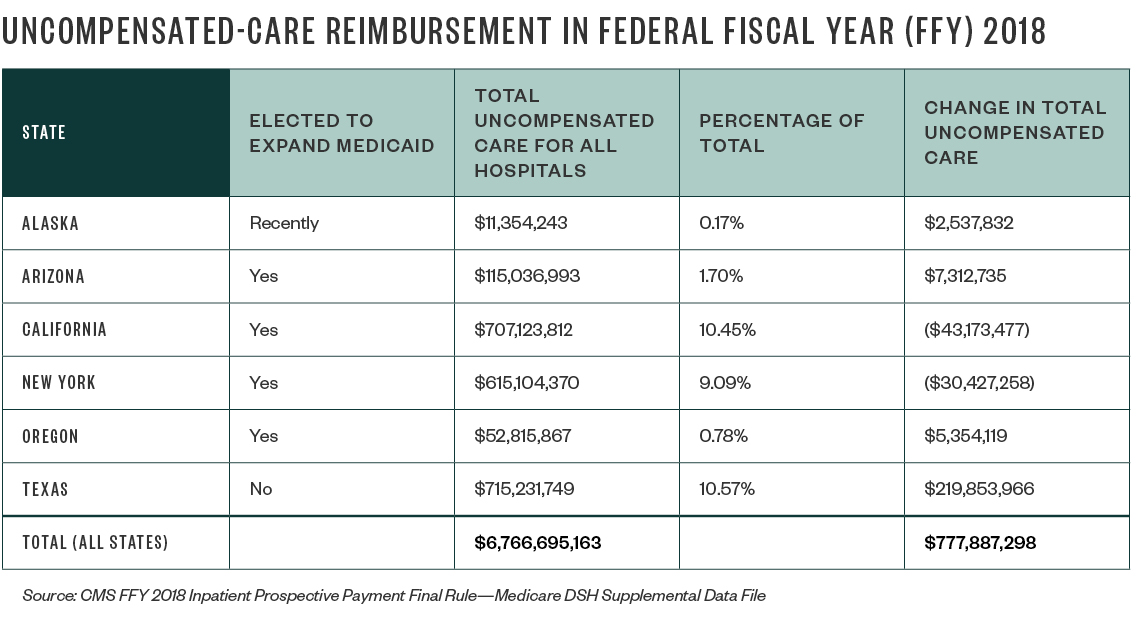
As the table above shows, Texas—a state that didn’t expand its Medicaid program—will be the largest beneficiary of this change, gaining a significant increase in its inpatient reimbursement. Hospitals in California and New York, on the other hand, will see declining reimbursement rates due to their Medicaid expansion and other factors.
Concerns
Many groups, including the American Hospital Association, American Federation of Hospitals, and Healthcare Financial Management Association, have provided CMS with written comments and concerns about the use of Worksheet S-10 data in calculating reimbursement for inpatient services. These concerns include the following:
- Unclear nature of the worksheet’s instructions
- Inconsistent nature in which hospitals apply their charity care policies nationwide, either due to organization type or varying demands of government bodies
- Worksheet data that hasn’t been audited by Medicare Administrative Contractors (MACs)
Commenters have emphasized that it’s especially unusual for CMS to overhaul payment methodologies using data that hasn’t been reviewed by a MAC or assessed by CMS for aberrations that may create issues down the line for hospitals.
Next Steps
Until January 2, 2018, hospitals eligible for a distribution from the uncompensated-care pool have the opportunity to review and revise their data for cost reporting periods beginning in 2014 and 2015 federal fiscal years.
Based on recent guidance from CMS, if hospitals are able to submit their revisions by December 2, 2017, any updates will be included in CMS’s proposed inpatient rulemaking for federal fiscal year 2019.
It’s important to note that this new process of reporting and review may trigger a MAC review or audit cycle—similar to the process involved in a wage index review—and that there may consequently be a large-scale shuffle in the monetary distributions that occur in the first few years that follow the review.
It’s still to be determined whether the uncompensated-care pool will help to close the gap between patient-care cost and reimbursement rates—or whether the ACA can create better coverage so that all patients pay something for their care. Only time will tell what the real impact of the ACA will be.
We’re Here to Help
For more information on the effect of the ACA on your hospital’s cost reimbursement model, contact your Moss Adams professional.